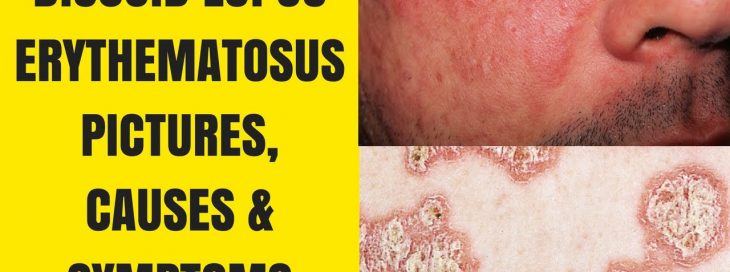
SEBACEOUS GRANULOMAS: A NOVEL FEATURE OF DISCOID LUPUS ERYTHEMATOSUS – CASE STUDY BY THE BEST SKIN SPECIALIST IN ISLAMABAD PAKISTAN
nternational Journal of Pathology; 2010; 8(1): 22-25 22
Original Article
Sebaceous Granulomas: A Novel Feature of Discoid Lupus Erythematosus
Rifat Yasmin, Dr. Ikramullah Khan, Anwar Ul Haque, Syed Afaq Ahmad
Objective: To determine the frequency of sebaceous granulomas formation in discoid lupus erythematosus.
Study Design: Retrospective observational study.
Setting: Departments of Dermatology and Pathology, Pakistan Institute of Medical Sciences, best skin specialist in islamabad.
Material and Methods: 100 cases of Discoid Lupus Erythematosus (DLE)spanning over two years and with the age range of 3 years to 70 years were examined for the presence of Sebaceous Granuloma. Other features of DLE like hyperkeratosis, follicular plugging, epidermal atrophy, basal layer vacuolization, basement membrane deposits, pigmentary incontinence, perivascular inflammation, periappendigeal inflammation, and collagen damage were also noted.
Introduction: Lupus erythematosus is an immune complex, type III hypersensitivity disease where antibodies are formed against native Deoxyribose Nucleic Acid (DNA). The immune compexes are deposited in various organs and various sites causing marked pleotropism. If several systems are involved then the disease is named Systemic Lupus Erythematosus (SLE) and if skin is exclusively involve the term Discoid Lupus Erythematosus (DLE) is used. One of the several features of DLE includes periappengeal inflammation. This may at times completely wipe out sebaceous glands forming sebaceous granulomas.
Results: Out of these 100 cases 8 cases contained sebaceous granulomas. These granulomas were composed of epithelioid cells, foreign body giant cells containing partially digested sebaceous material and a few lymphoctytes.
Conclusion: Sebaceous granulomas formation was seen in 8 % cases of discoid lupus erythematosus. This feature must be recognized both by dermatologists and pathologist so that diagnosis of DLE may not be distracted and erroneous diagnosis due to presence of granulomas may not be rendered.
Key Words: Discoid lupus erythematosus (DLE), Systemic Lupus Erythematosus (SLE), periappendageal inflammation, chronic granulomatous inflammation, sebaceous granulomas.
Introduction:
Discoid lupus erythematosus (DLE) is a chronic, scarring, atrophy producing, photosensitive dermatosis. Discoid lupus erythematosus may occur in patients with systemic lupus erythematosus (SLE), and some patients (<5%) with discoid lupus erythematosus progress to SLE.1 Some patients also have the lesions of subacute cutaneous lupus erythematosus (SCLE), and some may have a malar rash. Discoid lupus erythematosus lesions (DLE) are frequently fairly characteristic. The primary lesion is an erythematous papule or plaque with slight-to-moderate scaling. As the lesion progresses, the scale may thicken and become adherent, and pigmentary changes may develop. Patients with discoid lupus erythematosus rarely fulfil four or more of the criteria used to classify SLE.2Serologic abnormalities are uncommon.3 Therapy with sunscreens, topical corticosteroids, and antimalarial agents is usually effective. This study was based on hitherto undescribed sebaceous granulomas as a feature of DLE in some cases which we observed in our weekly dermatopathological conference held in our institution. The sebaceous granulomas are apparently formed due to destruction of sebaceous glands from intense chronic periappendigeal inflammation. The liberated lipid and fat vacuoles initiate and promote phagocytic activity, epithelioid cell differentiation and giant cell formation finally culminating into well formed granulomas. This feature was of course not seen in all cases but observed in some cases. The purpose of this study was to determine the frequency of the sebaceous granulomas and to create awareness among dermatologists and pathologists about this feature which may otherwise lead to erroneous diagnoses.

Figure I: DLE: Skin biopsy: Hyperkeratosis, keratin plugging, epidermal atrophy, basal cell vacuolization and several sebaceous granulomas (H& E X 100)
Materials and Methods
This prospective descriptive study was carried out at Pathology Department of Pakistan Institute of Medical Sciences(PIMS) based on our observations in weekly Dermato-Pathological conferences. 100 cases of DLE patients of both gender and age range of 3 years to 70 years, spanning over two years period were examined specifically for the presence or absence of well formed sebaceous granulomas. All cases with the clinical suspicion of cutaneous LE were biopsied, which were routinely processed and stained in the department of pathology using formalin fixation and hematoxylin and eosin (H&E) staining. The slides were seen jointly in the weekly Dermatopathology session held every Friday together with consultant pathologist along with the whole dermatology department on multihead microscope attached with TV monitors and overhead projector. We observed that along with usual hyperkeratosis, follicular plugging, epidermal atrophy, basal layer vacuolization, basement membrane deposits, pigmentary

Figure II: DLE: Skin biopsy: Sebaceous Granulomas with punched out lipid vacuoles. (H& E X 200)
incontinence perivascular inflammation, periappendigeal inflammation, and collagen damage, some cases had complete replacement of the sebaceous glands with their replacement with well formed sebaceous granulomas. All such cases were studied in detail toward composition and characteristic granulomas.
Results
Out of these 100 cases, 8 casescontained sebaceous granulomas. The cases were associated with absence of normal sebaceous glands. Remnants of hair follicles and/or erector pylorum muscles provided the clue to the true nature of the granulomas. These granulomas possessed macrophages containing large lipid vacuoles derived from sebaceous glands. Some of these macrophages converted into Langhan’s type multinucleated giant cells. (Figure I and II)
Other histopathological features included hyperkeratosis, keratin plugging, epidermal atrophy, basal cell vacuolization, perivasuclar inflammation, and collagen damage.(Table I)
| Histopathological feature | Percentage of patients |
| Hyperkeratosis | 100% |
| Parakeratosis | 20% |
| Follicular plugging | 65% |
| Epidermal atrophy | 97% |
| Acanthosis | 40% |
| Basal cell vacuolization | 100% |
| Pigmentary incontinence | 30% |
| Perivascular inflammation | 96% |
| Sebaceous granulomas | 94% |
| Periappendigeal inflammation | 8% |
| Collagen damage | 100% |
Table : I Frequency Table of histopathological features of patients
Discussion
Discoid lupus erythematosus is a chronic dermatological disease that can lead to scarring, hair loss, and hyperpigmentation changes in the skin if it is not treated early and promptly1 . It has a prolonged course and can have a considerable effect on quality of life. The prevalence is between 17 and 48 per 100,000 people. Women are affected about twice as often as men, compared with 10 times the frequency for SLE. The usual age of onset is between 20 and 40 years, which is about 20 years younger than SLE. Lupus erythematosus (LE) is thought to be an autoimmune disease which belongs to a group of connective tissue diseases like scleroderma, rheumatoid arthritis, polymyositis, and mixed connective tissue disease. Within the spectrum of diseases included in LE, at one end is a disease confined mainly to the skin and referred to as discoid lupus erythematosus (DLE) and at the other end is a florid disease with systemic involvement of heart, lungs, brain, kidneys and other organs called systemic lupus erythematosus (SLE). In between the two ends of the spectrum are disorders like subacute cutaneous lupus. Subacute cutaneous lupus erythematosus (SCLE) has a rather sudden onset with annular or psoriasiform plaques erupting on the upper trunk, arms, and/or dorsa of hands, usually after exposure to sunlight1. Although at the benign end of the spectrum, 1% to 5% of patients with discoid lupus may develop SLE and 25% of patients with SLE may develop typical chronic discoid lesions at some time during the course of their illness.2 Lupus occurs in all age groups with a mean age varying from 21 to 50 years1,2 and a prevalence of 17 to 48 in 100,000, with a greater prevalence in AfroCaribbean people. Although LE is an autoimmune disease, it is thought to result from interplay of certain genetic factors, environmental factors like ultraviolet light, and hormonal factors with antibodies.3 Early recognition and treatment improves the prognosis. The diagnosis is usually made by clinical examination. In some cases histopathology3 may be required to confirm the diagnosis. The histology is that of a lichenoid tissue reaction with changes at the dermo-epidermal junction that include thickening of the basement membrane (best demonstrated by periodic acid-Schiff staining) and vacuolar degeneration of the basal cells along with perivascular and periappendigeal inflammatory cell infiltration of a variable degree in the reticular dermis. Hyperkeratosis is more evident and follicular plugging may be seen in more mature lesions.4,5 DLE tends to run a less severe course than SLE and has a better prognosis.6 It is important for family physicians to recognize DLE because it is a potentially scarring disease. Early referral and institution of treatment by dermatologists increases the hope of minimizing the progression of the disease and consequent socioeconomic impact on the individual. There is insufficient evidence for the effective treatment. Because lesions are induced or exacerbated by ultraviolet exposure, photoprotective measures are important. Potent topical steroids and antimalarials are the mainstay of treatment. Some cases of discoid lupus erythematosus can be refractory to standard therapy; in these cases retinoids, thalidomide7 , and topical tacrolimus8 offer alternatives, as do immunosuppressives like azathioprine, cyclosporine, mycophenolate mofetil, and methotrexate.9 The histopathological features observed in discoid lupus erythematosus include vacuolar alteration of the basal cell layer, thickening of the basement membrane, follicular plugging, hyperkeratosis, atrophy of the epidermis, incontinence of pigment, and inflammatory cell infiltrate (usually lymphocytic) in a perivascular, periappendigeal, and sub epidermal location. Often, an abundance of mucin is seen within the dermis.10 The histopathological features differ depending upon the type and age of the lesion.11 In this study histopathological features were having hyperkeratosis, basal cell damage and collagen damage as most common features with presence in 100% of cases. Epidermal atrophy was seen in 97% of cases and periappendigeal and perivascular inflammation in 96% and 94% of patients respectively. Acanthosis was found in 40% of cases. Parakeratosis was the least found feature with percentage of only 20. (Table I) Total number of cases which were examined over period of two years was 100. Out of these 100 cases 8 cases showed formation of sebaceous granulomas.This finding has not previously been discussed much with the histopathological findings of discoid lupus erythematosus. Another important finding in this study was the earlier destruction of sebaceous glands than hair follicle. This was shown in the form of lymphocytic infiltration of sebaceous glands, disruption of glandular structure and formation of sebaceous granulomas comprising foreign body giant cells as well as partially digested sebaceous material. Skin is host to many different types of granulomas.12 Like tuberculosis and leprosy where the lipid coat of the Mycobacterium serve as an inciting factor, lipid of sebaceous gland may lead to granulomas formation. Granuloma formation may result from simple hemorrhages in some cases. (Cholesterol granuloma)13. Apart from infectious agents such as Leishmania Donovani bodies and Fungi, dead hair and myriad of foreign bodies may result in granuloma formation. Endogenous substances such as mammary gland secretions (granulomatous mastitis), sperm (spermatocytic granuloma), dead or damaged collagen (granuloma Annulare, cutaneous laxa) may result in granulomas formation. 14 Endogenous Hemorrhages (giant cell Tumour of bone) and in present study lipid of sebaceous glands may cause granuloma formation. Evaluation of each and every microscopic feature is necessary to further delineate the etiology and clinical course of the disease.15 More studies are needed to evaluate the changes on larger scale as this might be having some relationship to the duration or severity of clinical features of DLE and may be helpful in the treatment and prognosis of these patients.
Conclusion
Sebaceous granuloma formation is an important dermatopathological finding which can be occasionally encountered in DLE. Sebaceous glands seem to be destroyed earlier than the hair follicles and hence persisting hair follicles and erector pylorum muscle may provide a clue to the true nature of sebaceous granulomas. Both dermatologists and pathologists must be aware of this infrequent feature (8% in our study) in order not to be distracted from the diagnosis of DLE and from rending an erroneous diagnosis based on the granulomas.
References
1. Fabbri P, Cardinali C, Giomi B, Caproni M. Cutaneous lupus erythematosus: diagnosis and management. Am J Clin Dermatol 2003; 4: 449–65.
2. Weber F, Schmuth M, Fritsch P, Sepp N. Lymphocytic infiltration of the skin is a photosensitive variant of lupus erythematosus: evidence by phototesting. Br J Dermatol. 2001;144:292–296.
3. Crowson AN, Magro C. The cutaneous pathology of lupus erythematosus: a review. J Cutan Pathol. 2001;28:1–23.
4. Baima B, Sticherling M. Apoptosis in different cutaneous manifestations of lupus erythematosus. Br J Dermatol. 2001;144:958–966.
5. Parodi A, Caproni M, Cardinali C, et al.. Clinical, histological and immunopathological features of 58 patients with subacute cutaneous lupus erythematosus. Dermatology. 2000;200:6– 10.
6. Callen JP. Cutaneous lupus erythematosus: a personal approach to management. Australas J Dermatol. Feb 2006;47(1):13‐27.
7. Housman TS, Jorizzo JL, McCarty MA, Grummer SE, Fleischer AB Jr, Sutej PG. Low‐dose thalidomide therapy for refractory cutaneous lesions of lupus erythematosus. Arch Dermatol. Jan 2003;139(1):50‐4.
8. Heffernan MP, Nelson MM, Smith DI, Chung JH. 0.1% tacrolimus ointment in the treatment of discoid lupus erythematosus. Arch Dermatol. Sep 2005;141(9):1170‐ 1.
9. Wenzel J, Brahler S, Bauer R, Bieber T, Tuting T. Efficacy and safety of methotrexate in recalcitrant cutaneous lupus erythematosus: results of a retrospective study in 43 patients. Br J Dermatol. Jul 2005;153(1):157‐62.
10. AL, Venketaram MN, Bhushnurmath SR.Cutaneous lupus erythematosus:comparison of direct immunofluorescencefindings with histopathology.Int J Dermatol.1995;34:480‐2.
11. Jerdan MS, Hood AF, Moore GW, Callen JP. Histopathologic comparison of the subsets lupus erythematosus.Arch Dermatol 1990;126:52‐5.
12. Qureshi R, Shaikh R and Haque AU. Chronic granulomatous inflammatory disorders of skin at a tertiary care hospital in Islamabad. Int J Pathol 2004; (2) 31‐34
13. Haque AU In Situ hemorrhage Int. J Pathology 2003 (1) 60
14. Saeed M and Haque AU. Cutaneous laxa with granulomatous inflammation Int.J. Pathol 2008; 6 (2) 86‐90
15. Moatasim A and Haque AU The value of individual microscopic features in diagnosis of cutaneous lupus erythematosus. Int J Pathol 2005 3; 76‐80.
For Updates and Details Visit: www.drikram.comLike our Page
https://www.facebook.com/drikramullahkhanofficial/