Case Report – Granuloma Formation in Discoid Lupus Erythematosus: A Novel Microscopic Feature
Rifat Yasmin, Prof. Dr. Ikramullah Khan, Anwar Ul Haque, Syed Afaq Ahmad
Pakistan Institute of Medical Sciences, Islamabad : Sebaceous Granuloma Formation in Discoid Lupus Erythematosus
Abstract
Background: Lupus erythematosus is an autoimmune disease with diverse manifestations. When multiple systems are involved, it is termed systemic lupus erythematosus (SLE), while exclusive skin involvement is referred to as discoid lupus erythematosus (DLE). Periappendageal inflammation is a recognized histopathological feature of DLE, which can lead to the formation of sebaceous granulomas.
Objective: This study aims to determine the frequency of sebaceous granuloma formation in discoid lupus erythematosus.
Materials and Methods: A prospective observational study was conducted at Pakistan Institute of Medical Sciences, Islamabad. Over a span of two years, we examined 100 cases of DLE. We assessed histopathological features, including sebaceous granulomas, along with other common indicators of DLE.
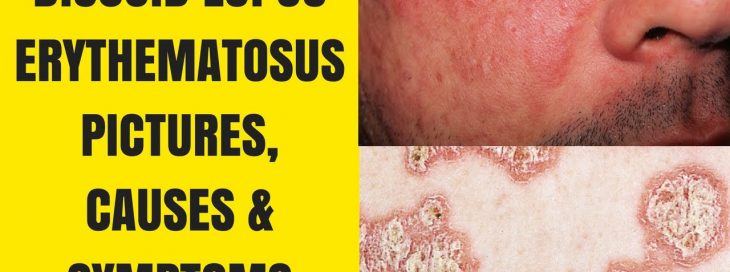
Results: Out of 100 cases, 8 exhibited sebaceous granulomas. These granulomas contained epithelioid cells, foreign body giant cells with digested sebaceous material, and lymphocytes.
Conclusion: Our findings highlight the presence of sebaceous granulomas in 8% of DLE cases. This unique feature must be understood by both dermatologists and pathologists to ensure accurate diagnosis and prevent misinterpretation due to the presence of granulomas.
Introduction
Discoid lupus erythematosus (DLE) is a chronic, atrophic, photosensitive skin disease. While DLE can coexist with systemic lupus erythematosus (SLE), they differ in severity and systemic involvement. DLE primarily affects the skin, and its primary lesion is an erythematous papule or plaque. Patients with DLE rarely fulfill criteria for SLE. Additionally, serologic abnormalities are uncommon. Nonetheless, treatment with sunscreens, topical corticosteroids, and antimalarial agents has proven effective. This study delves into a previously undescribed histopathological feature of DLE – the presence of sebaceous granulomas. These granulomas result from intense chronic periappendageal inflammation, which ultimately leads to the destruction of sebaceous glands.
Materials and Methods
For this observational study, we examined 100 DLE cases spanning two years. Our aim was to evaluate the presence of sebaceous granulomas, in addition to assessing other common histopathological features like hyperkeratosis, epidermal atrophy, perivascular inflammation, and collagen damage.
Results
Among the 100 cases, 8 cases exhibited sebaceous granulomas. These granulomas were characterized by epithelioid cells, foreign body-type giant cells, and lymphocytes. Furthermore, we observed typical features of DLE, such as hyperkeratosis, epidermal atrophy, and collagen damage.
Discussion
DLE can lead to various complications, including scarring, hair loss, and hyperpigmentation if not treated promptly. Its prevalence varies, affecting around 17 to 48 individuals per 100,000 people, with a higher incidence in women compared to men. DLE falls within the broader lupus spectrum, with DLE primarily affecting the skin and SLE involving multiple organs. Subacute cutaneous lupus erythematosus (SCLE) lies between these two extremes. In our study, we identified sebaceous granulomas as an important feature of DLE. These granulomas may originate from lipid destruction within sebaceous glands. The presence of lipid might initiate granuloma formation, a phenomenon observed in various contexts, including infections and foreign body reactions. Further investigation is warranted to understand the clinical implications of this unique finding.
Conclusion
In conclusion, our study revealed sebaceous granuloma formation in 8% of DLE cases. Recognizing this distinct feature is vital for dermatologists and pathologists alike. It ensures accurate diagnosis, preventing misinterpretation due to the presence of granulomas, and contributes to improved patient management and outcomes.
Address for Correspondence:
Dr. Rifat Yasmin, Department of Dermatology, Pakistan Institute of Medical Sciences, Islamabad. E-mail: rifat_chaudhary@yahoo.com





 Humidity Gadge
Humidity Gadge A Humidifier
A Humidifier







 Figure 4: A hostopathology sample showing Multiple Giant Cells and Granulomas
Figure 4: A hostopathology sample showing Multiple Giant Cells and Granulomas